Peripheral Arterial Disease or PAD is the form of cardiovascular disease. This disease affects the blood vessels that are located outside of the brain and heart. PAD is often confused with the Peripheral Vascular Disease or PVD. However, Peripheral Arterial Disease affects the arteries whereas Peripheral Vascular Disease or PVD affects the arteries and veins. These two terms are often used interchangeably.
Peripheral arterial disease (PAD) is generally associated with blocked arteries in the arms and legs. However, it can also affect the arteries of other regions as well that carry oxygen-rich blood to arms, stomach, and kidneys. When the arteries of the legs are affected, the ability to walk can be impaired, and the blockage can cause severe pain, swelling or even death.
Peripheral Arterial Disease occurs when the normal blood flow is restricted due to the plaque build-up in the arteries. This causes a blocked blood flow that results in pain and numbness in the legs. If not treated, this disease can cause severe complications and may even lead to leg amputation.
PAD generally affects older people, however, people who are diagnosed with heart-related problems and who smoke, or had a history of smoking are equally likely to get affected from this disease.
Causes of Peripheral Arterial Disease
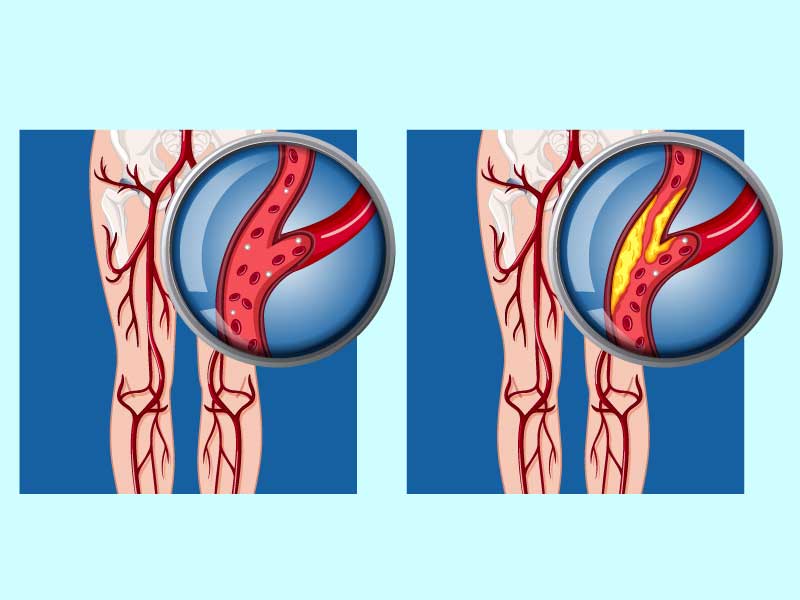
PVD, including PAD, can be a consequence of atherosclerosis, an inflammatory disease that leads to narrowing of blood vessels. This can be caused by atherosclerosis (hardening of the arteries) and causes blood vessel spasms. It is usually caused by the lack of blood supply in the legs and feet, but can also cause pain and fatigue in other limbs. While discussions about atherosclerosis usually focus on the heart, the disease can affect any artery in the body.
If a person is overweight or inactive or has a history of heart disease, diabetes, high blood pressure or high cholesterol, he/she may be at risk for PAD.
PAD is closely linked to heart disease, high blood pressure and high cholesterol, as well as obesity and diabetes.
People who smoke have a higher risk of developing peripheral arterial diseases due to reduced blood circulation. The narrowing of a blood vessel due to plaque build-up can lead to reduced blood flow to the extremities and hence can cause PAD.
Symptoms of Peripheral Arterial Disease

“Intermittent Claudication” is a common symptom of peripheral arterial disease. PAD most commonly affects the legs, and depending on where the blockage is in the leg arteries, it can affect the feet, calves, thighs, and buttocks. A person with PAD may experience pain and heaviness in the leg while walking or climbing stairs because blood flow to the limbs is no longer sufficient to keep up with demand.
Other signs may include:
- Weak pulse in the legs
- Pale or bluish skin color
- Wounds and sores in the leg that do not heal properly
- Difference in temperature between the two legs
- Erectile dysfunction in men
Prolonged pain or discomfort in the legs is also a sign of this disease.
Diagnosis of Peripheral Arterial Disease

There are several ways by which PAD can be diagnosed, which includes studying about the family history, a physical examination, and the test results.
Ankle-Brachial Index
In this test, which takes about 10 to 15 minutes, the Ankle-Brachial Index (ABI) is identified by comparing the blood flow in the arms with the blood flow in the legs. A normal ABI is 1.0 or greater (ranging from 0.90 to 1.30). The difference in the blood flow can determine if the arteries are blocked and to what extent.
Doppler Ultrasound
Doppler Ultrasound determines the blood flow in the primary arteries and veins in the limbs. In this test, a device is placed onto the body and moved back and forth to analyse the difference in blood flow in the arteries of the affected area. The device identifies the sound waves of the blood flow and converts that into the picture that shows the blood flow in the arteries.
Computer Tomographic Angiography (CT)
A non-invasive test that involves imaging of the arteries of the abdomen, pelvic, and leg region of the patient. This test is generally useful for the people with pacemakers and stents.
Treadmill Test
During this test, the patient is made to walk on the treadmill. The ABI testing is done before and after the walking exercise is done to determine the difference of the physical activity on the blood flow of the arteries.
This test focuses on knowing if the strenuous activity affects the blood flow in the artery and if yes, then up to what extent.
Magnetic Resonance Angiogram (MRA)
This test uses magnetic and radio waves to image the blood vessels. This test is similar to the Magnetic Resonance Imaging (MRI). In the imaging, doctors usually can identify the location and severity of the blocked blood vessel.
Arteriogram
Arteriogram is the type of test that provides a kind of road map of the arteries. In this type of test, the dye is injected into the arteries through a catheter tube or a needle. After that, an X-Ray imaging is done. This is helpful in identifying the location and extent of the blockage in the artery.
Blood Tests
Some doctors recommend blood tests to check for PAD as blood tests can help identify other diseases such as diabetes and high cholesterol.
Takeaway
Peripheral arterial disease (PAD) is a blood circulation problem that causes narrowing of the arteries that reduces blood flow to the extremities of the body. It is also likely to cause heart failure, stroke, heart attack, and stroke. If a person develops peripheral artery disease or PAD, the extremities, usually legs, do not receive enough blood to keep up with demand. Typically it causes pain and fatigue, often in both legs and especially during exercise.
People who are diagnosed with PAD are at a higher risk of ischemic heart disease, stroke, and even heart attack.
It is always recommended to consult the general physician or family doctor in case people feel any numbness or weakness in the legs frequently.